CEO SUMMARY: Deteriorating finances at many rural hospitals and smaller community hospitals is a growing trend. It is also a new consulting opportunity for local pathologists because financially-strapped hospitals often give their labs inadequate working capital and lack the staff needed to comply fully with state and federal compliance requirements. In Shreveport, Louisiana, Delta Pathology …
Pathologists Benefit from Hospital Lab Consulting Read More »
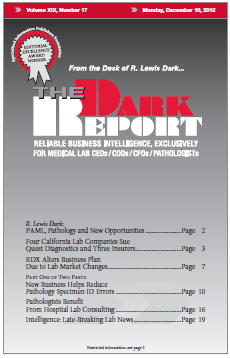
To access this post, you must purchase The Dark Report.