CEO SUMMARY: Allegations of anticompetitive and monopolistic behaviors that violate state and federal laws are the basis of a private lawsuit filed by four independent clinical lab companies in California. The defendants are Quest Diagnostics Incorporated, Aetna, Blue Shield of California, and the Blue Cross Blue Shield Association. Plaintiffs claim that the defendants “conspired… to …
Four California Labs Sue Quest and Three Insurers Read More »
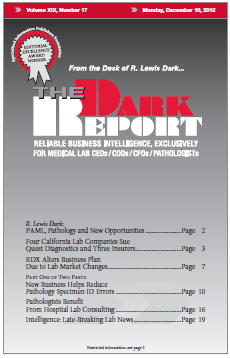
To access this post, you must purchase The Dark Report.