CEO SUMMARY: When pathology labs discover instances of a misidentified or contaminated tissue specimen, there is a new service that allows them to retrospectively use DNA to properly match that specimen to the correct patient. In part two of our series, we look at how some pathology labs are using the Know Error service to …
Pathology Labs Want Method To Correct Specimen ID Errors Read More »
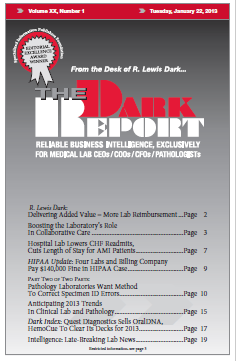
To access this post, you must purchase The Dark Report.