CEO SUMMARY: As healthcare transitions away from fee-for-service payment and adopts new models of reimbursement, every clinical lab will need to deliver more value with its lab testing services. At Henry Ford Health System in Detroit, the laboratory division has blazed a path of improving lab performance specifically to enable it to add value to …
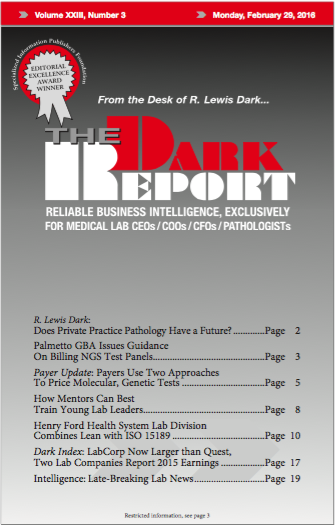
Henry Ford Health System Laboratory Division Combines Lean with ISO 15189 Read More »
To access this post, you must purchase The Dark Report.