PRIVATE PAYERS AND MEDICARE contractors are taking divergent approaches to establishing coverage policies and setting prices for molecular and genetic tests. That’s what Kuo Bianchini Tong, MS, CEO of Quorum Consulting Inc., sees happening. “One approach seeks to recognize the clinical utility and value of these tests with nuanced, more discreet coding and pricing,” he …
Payers Using Two Approaches To Price Molecular, Genetic Tests Read More »
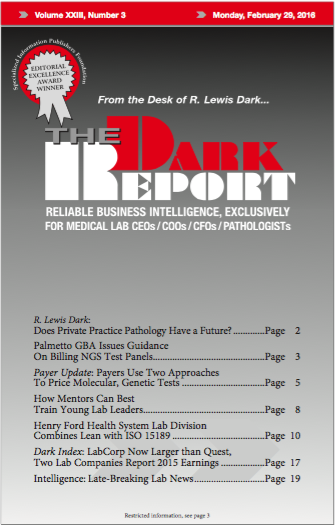
To access this post, you must purchase The Dark Report.