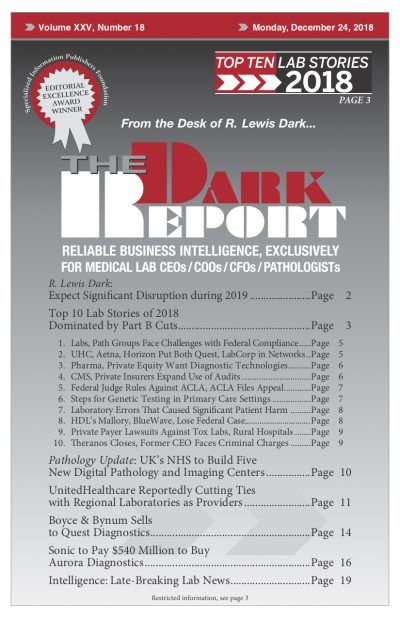
CEO SUMMARY: This year’s list of the Top 10 Lab Industry Stories for 2018 is dominated by new directives from Medicare and private health insurers, as well as significant decisions by federal courts. Collectively, these developments create new compliance risks for all clinical laboratories and anatomic pathology groups. What is more notable about these top …
Several Big Surprises in 2018’s Top 10 Lab Stories Read More »
To access this post, you must purchase The Dark Report.