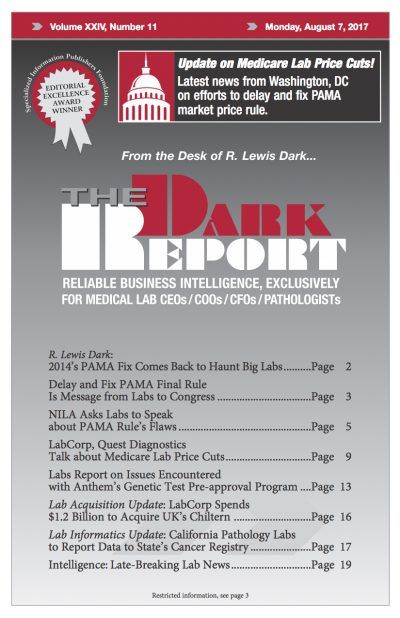
CEO SUMMARY: In a call to action, the National Independent Laboratory Association is urging lab owners, lab managers, and pathologists to educate their members of Congress about the biases and deep flaws built into the final rule for PAMA market price reporting and how the rule will result in reduced access to clinical lab testing …
NILA Asks Labs to Speak about PAMA Rule’s Flaws Read More »
To access this post, you must purchase The Dark Report.