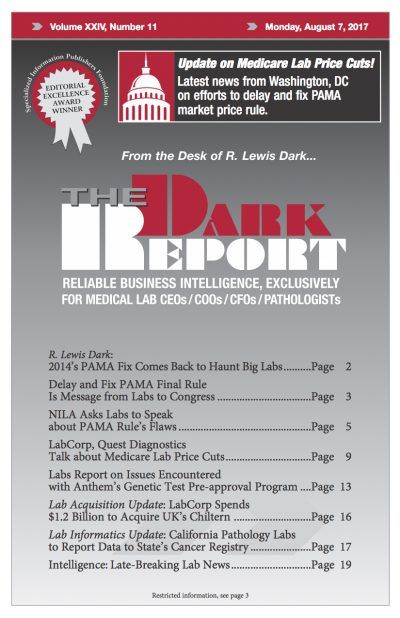
CEO SUMMARY: Only a few months remain before the federal Centers for Medicare and Medicaid Services makes deep price cuts to Medicare Part B clinical laboratory test fees. Before those cuts go into effect, lab associations and lab professionals are educating members of Congress and the new administration about the bias and flaws in CMS’ […]
To access this post, you must purchase The Dark Report.