CEO SUMMARY: Since Anthem and AIM Specialty Health began a prior-authorization program for genetic testing July 1, a Northeast lab has not had any genetic tests approved through the new system. Physicians told the lab that the steps required for prior authorization were disruptive. Those doctors who regularly order genetic tests had not been trained …
Issues Encountered with Anthem’s Pre-approval Read More »
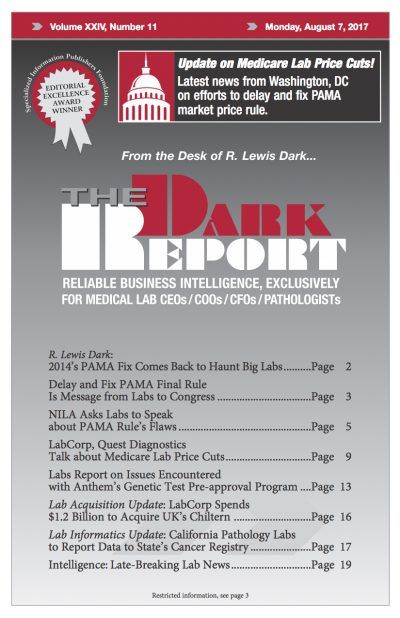
To access this post, you must purchase The Dark Report.