USE OF LEAN METHODS HAS UNLOCKED major improvements at Baystate Health’s Department of Pathology in Springfield, Massachusetts. One Lean project cut average Pap test turnaround time by more than 50%. Another Lean project attacked errors with Advanced Beneficiary Notices (ABN), leading to a 75% reduction in write-offs, worth $1 million! In the first case, the …
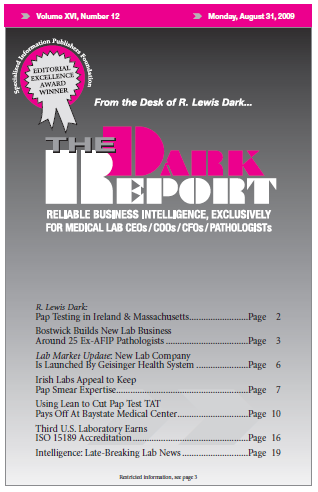
Using Lean to Cut Pap Test TAT Pays Off At Baystate Medical Read More »
To access this post, you must purchase The Dark Report.