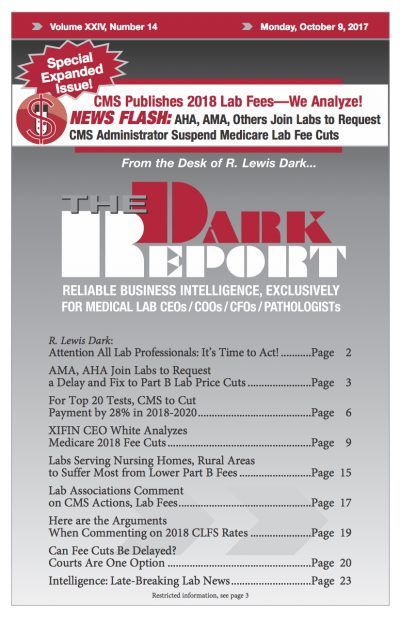
CLINICAL LABORATORIES WITH A HIGH percentage of Medicare Part B lab test reimbursement are expected to suffer the most under the Part B Clinical Laboratory Fee Schedule (CLFS) cuts that the Centers for Medicare and Medicaid Services proposed Sept. 22. With the proposed rates scheduled to go into effect on Jan. 1, that leaves just …
Labs Serving Nursing Homes, Rural Areas to Suffer Most Read More »
To access this post, you must purchase The Dark Report.