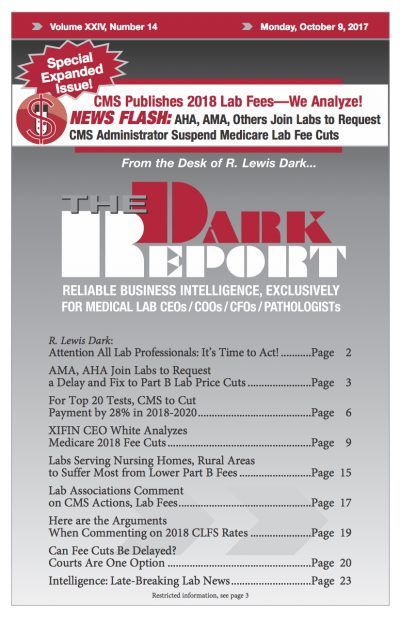
CEO SUMMARY: If the draft lab rates that CMS published Sept. 22 for the Clinical Laboratory Fee Schedule for 2018 go into effect Jan. 1 as proposed, then clinical labs will see a cut of 28% in what they get paid for the top 20 most common tests, according to a recent analysis. The rates …
XIFIN CEO White Analyzes Medicare 2018 Fee Cuts Read More »
To access this post, you must purchase The Dark Report.