TAG:
Clinical Laboratory Fee Schedule
Outpatient clinical laboratory services are paid based on the Medicare Part B Clinical Laboratory Fee Schedule (CLFS) in accordance with Section 1833(h) of the Social Security Act. Payment is the lesser of the amount billed, the local fee for a geographic area, or a national limit. In accordance with the statute, the national limits are set at a percent of the median of all local fee schedule amounts for each laboratory test code. Each year, fees are updated for inflation based on the percentage change in the Consumer Price Index. However, legislation by Congress can modify the update to the fees.
Co-payments and deductibles do not apply to services paid under the Medicare clinical laboratory fee schedule.
Each year, new laboratory test codes are added to the clinical laboratory fee schedule and corresponding fees are developed in response to a public comment process. Also, for a cervical or vaginal smear test (Pap smear), the fee cannot be less than a national minimum payment amount, initially established at $14.60 and updated each year for inflation.
Critical access hospitals are paid for outpatient laboratory services on a reasonable cost basis, instead of by the fee schedule. Hospitals with fewer than 50 beds in qualified rural areas—those with population densities in the lowest quartile of all rural areas—are paid based on a reasonable cost basis for outpatient clinical laboratory tests for cost reporting periods between July 2004 and July 2006.
The Protecting Access to Medicare Act of 2014 (PAMA) that became law on April 1, 2014, required labs to report such data and the test volumes associated with that data, beginning on Jan. 1, 2016.
On Jan. 1, 2017, CMS will use the market data to set prices for the Part B Clinical Laboratory Fee Schedule. As currently written, PAMA specifies that CMS cannot cut the price of a specific lab test by more than 10% in each of 2017, 2018, and 2019, nor by more than 15% in each of 2020, 2021, and 2022. There is no limit on price reductions outlined in the law for years following 2022.
Some Labs Performing ADLTs May See Increased Medicare Fees
By Joseph Burns | From the Volume XXIV No. 15 – October 30, 2017 Issue
MIXED IN THE BAD NEWS concerning the proposed Clinical Laboratory Fee Schedule for 2018, there is some good news regarding what the federal Centers for Medicare and Medicaid Services proposes to pay for certain advanced diagnostic tests. After analyzing the proposed fee schedule, …
XIFIN CEO WHITE ANALYZES MEDICARE 2018 FEE CUTS
By R. Lewis Dark | From the Volume XXIV No. 14 – October 9, 2017 Issue
CEO SUMMARY: If the draft lab rates that CMS published Sept. 22 for the Clinical Laboratory Fee Schedule for 2018 go into effect Jan. 1 as proposed, the…
Looming CMS lab fee schedule cuts unite AMA, AHA and labs in opposition
By Mary Van Doren | From the Volume XXIV No. 14 – October 9, 2017 Issue
This is an excerpt from a 1,237-word article in the Oct. 8, 2017 issue of THE DARK REPORT. The complete article is available for a limited time to all readers, and available at all times to paid members of the Dark Intelligence Group. CEO SUMMARY: In what m…
Attention All Lab Professionals: It’s Time to Act!
By R. Lewis Dark | From the Volume XXIV No. 14 – October 9, 2017 Issue
AT THIS MOMENT, THE ENTIRE CLINICAL LABORATORY INDUSTRY STANDS on the precipice of the most financially disruptive development in the past three decades. On Jan. 1, the federal Centers for M…
AMA, AHA Join Labs to Request Delay, Fix
By Robert Michel | From the Volume XXIV No. 14 – October 9, 2017 Issue
CEO SUMMARY: In what may be a first for the clinical lab industry, the American Medical Association and the American Hospital Association joined with 20 other healthcare associations to ask CMS Administrator Seema Verma to address the problems with the CMS proposal involving Medicare Part B f…
For Top 20 Tests, CMS to Cut Payment by 28% in 2018-2020
By Robert Michel | From the Volume XXIV No. 14 – October 9, 2017 Issue
ON SEPT. 22, MEDICARE OFFICIALS RELEASED THE DRAFT PRICES for the 2018 Clinical Laboratory Fee Schedule. The bad news for the lab industry is that the fee cuts are deeper than the federal Centers for Medicare and Medicaid Services had predicted earlier. The price cuts to clinical la…
XIFIN CEO White Analyzes Medicare 2018 Fee Cuts
By R. Lewis Dark | From the Volume XXIV No. 14 – October 9, 2017 Issue
CEO SUMMARY: If the draft lab rates that CMS published Sept. 22 for the Clinical Laboratory Fee Schedule for 2018 go into effect Jan. 1 as proposed, then clinical labs will see a cut of 28% in what they get paid for the top 20 most common tests, according to a recent analysis. The rates t…
Labs Serving Nursing Homes, Rural Areas to Suffer Most
By Joseph Burns | From the Volume XXIV No. 14 – October 9, 2017 Issue
CLINICAL LABORATORIES WITH A HIGH percentage of Medicare Part B lab test reimbursement are expected to suffer the most under the Part B Clinical Laboratory Fee Schedule (CLFS) cuts that the Centers for Medicare and Medicaid Services proposed Sept. 22. With the proposed rates schedul…
Lab Associations Comment on CMS Actions, Lab Fees
By Robert Michel | From the Volume XXIV No. 14 – October 9, 2017 Issue
FOR THE LAB INDUSTRY, THE FEE CUTS proposed in the 2018 Clinical Laboratory Fee Schedule would be even more aggressive than what the federal Centers for Medicare and Medicaid Services had earlier predicted for Medicare Part B. In the days following the Sept. 22 publication of the pr…
Here Are the Arguments When Commenting on 2018 CLFS Rates
By Joseph Burns | From the Volume XXIV No. 14 – October 9, 2017 Issue
ALL LABORATORY PROFESSIONALS AND pathologists are encouraged to submit comments to CMS before the Oct. 23, as well as send letters to their elected officials in Congress to urge both to delay and to fix the market price study and revise the proposed Clinical Laboratory Fee Schedule for 2018. Bene…
CURRENT ISSUE
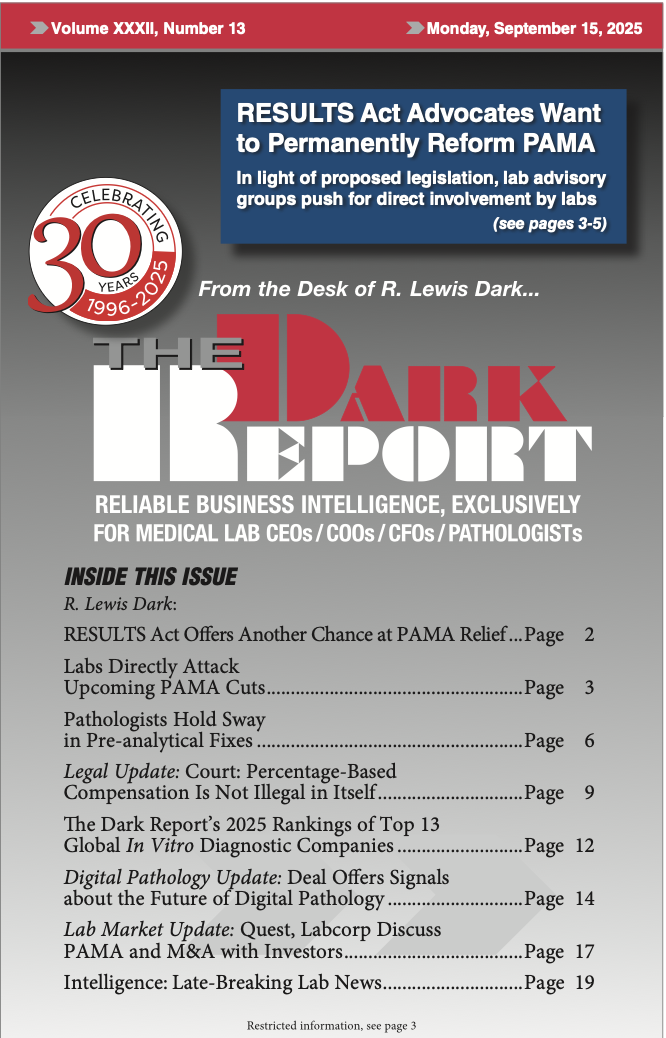
Volume XXXII, No. 13 – September 15, 2025
The Dark Report examines a new bill that would reform PAMA and avoid reimbursement rate cuts scheduled for January 2026. Clinical laboratory leaders are urged to make their voices heard in Congress. Also, an expert describes how labs can fix pre-analytical errors and avoid disaster.
See the full table of contentsHow Much Laboratory Business Intelligence Have You Missed?
Lab leaders rely on THE DARK REPORT for actionable intelligence on important developments in the business of laboratory testing. Maximize the money you make-and the money you keep! Best of all, it is released every three weeks!
Sign up for TDR Insider
Join the Dark Intelligence Group FREE and get TDR Insider FREE!
Never miss a single update on the issues that matter to you and your business.
Topics
- Anatomic Pathology
- Clinical Chemistry
- Clinical Laboratory
- Clinical Laboratory Trends
- Digital Pathology
- Genetic Testing
- In Vitro Diagnostics
- IVD/Lab Informatics
- Lab Intelligence
- Lab Marketplace
- Lab Risk & Compliance
- Laboratory Automation
- Laboratory Billing
- Laboratory Compliance
- Laboratory Equipment
- Laboratory Information Systems
- Laboratory Management
- Lean Six Sigma
- Managed Care Contracts
- Molecular Diagnostics
- Pathology Trends
- People
- Uncategorized

