CEO SUMMARY: As 2016 approaches, nearly every lab organization is watching and waiting to learn how federal regulators at CMS and the FDA will move forward with plans to implement PAMA market reporting and regulation of laboratory-developed tests, respectively. Most knowledgeable observers expect that each government program will cost labs substantial amounts of money—from fee …
Coming Next Year for Labs: PAMA, FDA, LDTs, and More Read More »
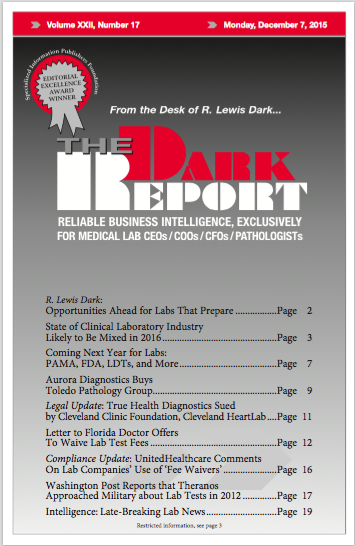
To access this post, you must purchase The Dark Report.