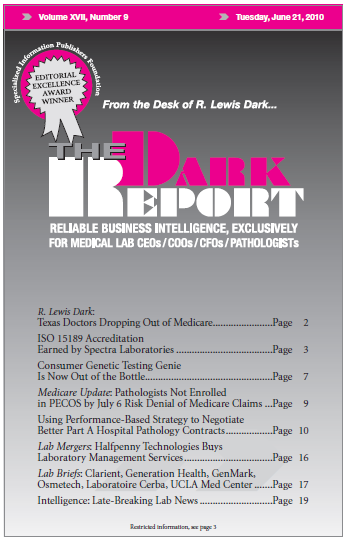
CEO Summary: One of pathology’s greatest challenges is adequate reimbursement for hospital Part A Pathology Services. Over the past two decades, ever more hospitals took steps to reduce or eliminate payment to pathologists for these services. Now several innovative pathology groups are using a performance-based strategy to negotiate win-win Part A Pathology Service contracts with …
Using Performance-Based Part A Hospital Path Contracts Read More »
To access this post, you must purchase The Dark Report.