CEO SUMMARY: Blue Cross Blue Shield of Tennessee has notified physicians that, starting January 1, it will reduce what it pays for lab testing to 52% of Medicare fees. Officials with the state medical association have been unable to get definitive answers to questions about what tests would be affected. Medicare officials have said consistently …
Tennessee BCBS Cuts Lab Fees to 52% of Medicare Read More »
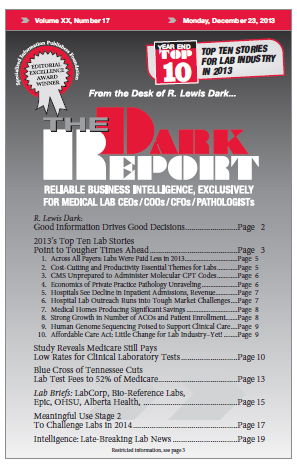
To access this post, you must purchase The Dark Report.