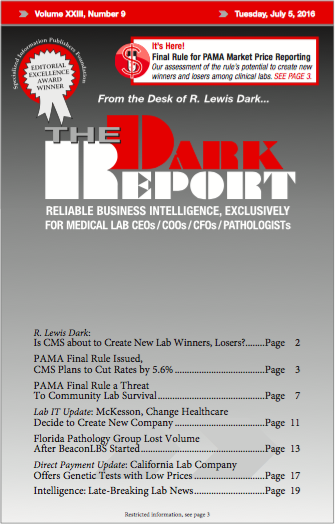
CEO SUMMARY: CMS issued its final rule for implementing the laboratory payment reform included in the Protecting Access to Medicare Act of 2014 (PAMA) on June 17. All labs will see significant reductions to the Medicare Part B Clinical Laboratory Fee Schedule that becomes effective on Jan. 1, 2018. That same section of PAMA requires …
PAMA Final Rule Issued, CMS Plans to Cut Rates by 5.6% Read More »
To access this post, you must purchase The Dark Report.