CEO SUMMARY: This will be one of the most challenging years facing the clinical lab industry since the early 1990s, when closed panel HMOs were the disruptive force that generated deep cuts in lab test prices. However, unlike HMOs of that era, the CMS scheme to collect private payer lab test prices and use that …
Why PAMA May Be Poised to Disrupt Lab Industry Read More »
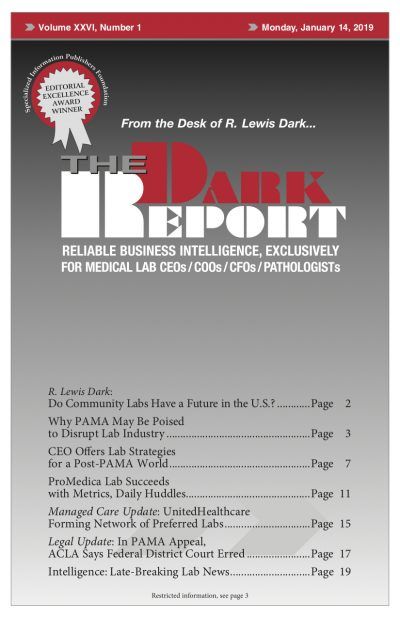
To access this post, you must purchase The Dark Report.