IN JUST SEVEN MONTHS, the age of accountable care organizations (ACO) begins. On January 1, 2012, the Centers for Medicare and Medicaid Services (CMS) will commence contracting with ACOs. ACOs are one of the major reforms spelled out in the 2,700-page health reform law that President Obama signed into law on March 23, 2010. Thus, …
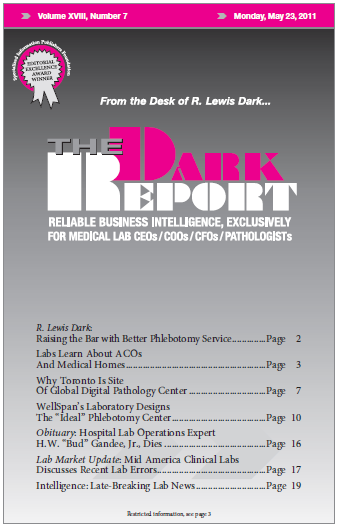
Labs Learn About ACOs And Medical Homes Read More »
To access this post, you must purchase The Dark Report.