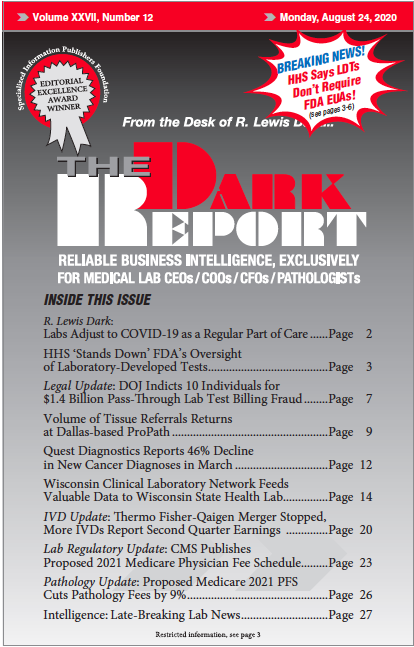
This is an excerpt of a 2,029-word article in the August 24, 2020 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. CEO SUMMARY: A directive from the federal Department of Health and Human Services (HHS) may have long-lasting implications for the federal Food and Drug Administration’s efforts …
FDA Will Have No Authority Over Laboratory-Developed Tests, HHS Says Read More »
To access this post, you must purchase The Dark Report.