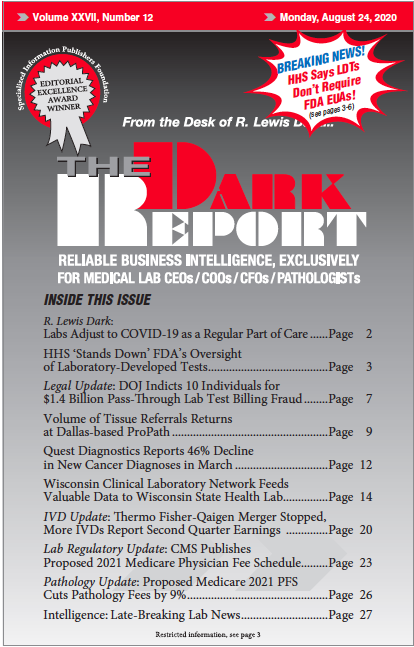
CEO SUMMARY: A directive from the federal Department of Health and Human Services (HHS) may have long-lasting implications for the federal Food and Drug Administration’s efforts to assert regulatory oversight of laboratory-developed tests (LDTs). In a statement last week, HHS said that labs “are not required” to obtain an FDA emergency use authorization or FDA clearance of LDTs. Clinical labs welcomed […]
To access this post, you must purchase The Dark Report.