IF THE PROPOSED MEDICARE 2012 PHYSICIAN FEE SCHEDULE (PFS) RULE—published by the Centers for Medicare and Medicaid Services (CMS) on Aug. 4—takes effect as currently written, pathology professional fees will be cut by 9%, effective Jan. 1, 2021. This was not welcome news for the anatomic pathology profession. The proposed 9% cut to Medicare payment for pathology services is the result of CMS deciding …
Proposed Medicare 2021 PFS Cuts Pathology Fees by 9% Read More »
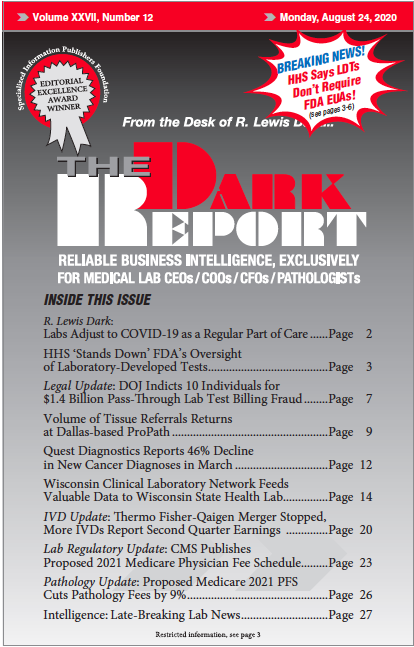
To access this post, you must purchase The Dark Report.