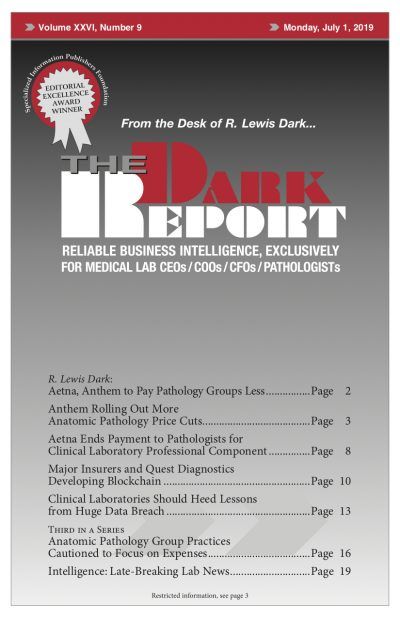
This is a synopsis of a 2,120-word article in the July 1, 2019 issue of THE DARK REPORT (TDR). The full articles are available to members of The Dark Intelligence Group. CEO SUMMARY: Anthem is making big changes to its relationships with anatomic pathology (AP) groups. Getting most of the attention at the moment are …
Anthem Rolling Out New Pathology CPT Code Cuts Read More »
To access this post, you must purchase The Dark Report.