CEO SUMMARY: As of Aug. 1, Aetna will stop paying out-of-network pathologists for the professional component review of certain clinical pathology tests. Until now, the health insurer has paid for the professional component when out-of-network labs billed for clinical lab tests using the modifier 26. In a notice to labs, Aetna said it will pay …
Aetna Ends Payment for Professional Component Read More »
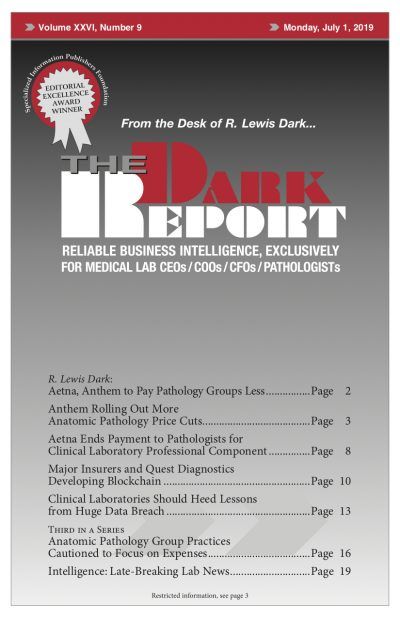
To access this post, you must purchase The Dark Report.