TAG:
Bundled payment
Bundled payment, also known as episode-based payment, episode payment, episode-of-care payment, case rate, evidence-based case rate, global bundled payment, global payment, package pricing, or packaged pricing, is defined as the reimbursement of health care providers (such as hospitals and physicians) “on the basis of expected costs for clinically-defined episodes of care.” It has been described as “a middle ground” between fee-for-service reimbursement (in which providers are paid for each service rendered to a patient) and capitation (in which providers are paid a “lump sum” per patient regardless of how many services the patient receives).
Advocates of bundled payments note that unlike fee-for-service, bundled payment discourages unnecessary care, encourages coordination across providers, and potentially improves quality. Unlike capitation, bundled payment does not penalize providers for caring for sicker patients. Bundling payment provides additional advantages to providers and patients alike, through removing inefficiency and redundancy from patient-care protocols; e.g. duplicate testing, delivering unnecessary care, and failing to adequately provide postoperative care.
This method of payment is also said to provide transparency for consumers by fixing pricing and publishing cost and outcomes data. Patients would be able to choose a provider based on a comparison of real data, not word of mouth. Bundled payments may also encourage economies of scale – especially if providers agree to use a single product or type of medical supply – as hospitals or integrated health systems can often negotiate better prices if they purchase supplies in bulk.
On the other hand, the scientific evidence in support of it has been described as “scant.” It does not discourage unnecessary episodes of care; for example, physicians might hospitalize some patients unnecessarily.
Providers may seek to maximize profit by avoiding patients for whom reimbursement may be inadequate (e.g., patients who do not take their drugs as prescribed), by overstating the severity of an illness, by giving the lowest level of service possible, by not diagnosing complications of a treatment before the end date of the bundled payment, or by delaying post-hospital care until after the end date of the bundled payment.
Meanwhile, early evidence indicates that Medicare’s bundled-payment pilot, the Bundled Payment Care Initiative, has helped participating providers improve the quality of care while better managing healthcare costs. Should more detailed findings confirm these outcomes, Medicare could decide to expand the range of clinical services it wants covered by a bundled-payment arrangement.
COLA: GAO Should Address PAMA’s Effect on Patients
By Joseph Burns | From the Volume XXVI No. 4 – March 18, 2019 Issue
CEO SUMMARY: In a recent statement, COLA, an organization that accredits clinical labs, expressed strong concern about how a report from the Government Accountability Office did not address how the Protecting Access to Medicare Act of 2014 (PAMA) affects patients’ access to testing, esp…
Project Santa Fe Labs Deliver Value with Tests
By Joseph Burns | From the Volume XXV No. 16 – November 13, 2018 Issue
CEO SUMMARY: No bigger threat looms over the financial security of the nation’s clinical laboratories than healthcare’s transition from fee-for-service payment to value-based reimbursement. To navigate that transition successfully, medical labs and pathology groups will need to adopt …
In Lawsuit Against HHS, ACLA Has Strong Positions
By Joseph Burns | From the Volume XXV No. 9 – June 18, 2018 Issue
CEO SUMMARY: Rulings from Judge Amy Berman Jackson of the U.S. District Court in Washington, D.C., are expected soon in the ACLA’s lawsuit against HHS concerning the PAMA final rule that set the course for the new Medicare CLFS rates implemented in January 2018. One lawyer following the…
Georgia Micro Lab Slashes TAT by Almost Two Days
By Joseph Burns | From the Volume XXV No. 6 – April 16, 2018 Issue
CEO SUMMARY: Two projects to boost the performance of the microbiology laboratory at University Health Services in Augusta, Ga., significantly reduced test turnaround times in ways that contributed to improved patient outcomes. The first project was in 2016, when the lab introduced mass s…
NILA Asks Labs to Speak about PAMA Rule’s Flaws
By Joseph Burns | From the Volume XXIV No. 11 – August 7, 2017 Issue
CEO SUMMARY: In a call to action, the National Independent Laboratory Association is urging lab owners, lab managers, and pathologists to educate their members of Congress about the biases and deep flaws built into the final rule for PAMA market price reporting and how the rule will resul…
CEO Describes Characteristics Of the Clinical Lab 2.0 Model
By Joseph Burns | From the Volume XXIV No. 7 – May 15, 2017 Issue
CEO SUMMARY: Moving away from volume-based care will not be easy for clinical labs. After all, high volume sustains labs. But labs seeking to transition away from fee-for-service to value-based care must have a seat at the table where decisions are made, said a lab CEO who is part of Proj…
LabCorp, Quest, Sonic Do Hospital Lab Deals
By Joseph Burns | From the Volume XXIV No. 4 – March 13, 2017 Issue
CEO SUMMARY: Is the New Year’s spate of deals involving the sales of hospital lab outreach programs and a new joint venture the first tremors of an impending earthquake of similar transactions? In the first 10 weeks of 2017, Laboratory Corporation of America, Quest Diagnostics, and Soni…
University of Michigan Pathologists Bet on Patient-Centered Care
By Joseph Burns | From the Volume XXIV No. 3 – February 21, 2017 Issue
CEO SUMMARY: At the University of Michigan Medical Center, the Department of Pathology is learning new ways to add value that include face-to-face meetings with patients as part of UMMC’s patient- and family-centered care initiative. One lesson learned is that patients appreciate the op…
Labs Discover Much Complexity In Their Lab Test Price Data
By Joseph Burns | From the Volume XXIII No. 16 – November 28, 2016 Issue
DON’T EXPECT IT TO BE EASY AND STRAIGHTFORWARD when reporting the prices of chemistry panels as the final rule for lab test market price reporting rule requires. Instead, labs should expect the process to be complex and troublesome. Also, labs should be concerned that Medicare officials have threa…
Medicare Part B Lab Test Prices Versus Budgeted Payment
By R. Lewis Dark | From the Volume XXIII No. 15 – November 7, 2016 Issue
THERE IS AN IMPORTANT QUESTION THAT lab industry magazines and news sources have failed to address: How many years are left before Medicare officials drop fee-for-service payment for clinical lab testing? On January 26, 2015, the Department of Health and Human Services (HHS) issued a press rele…
CURRENT ISSUE
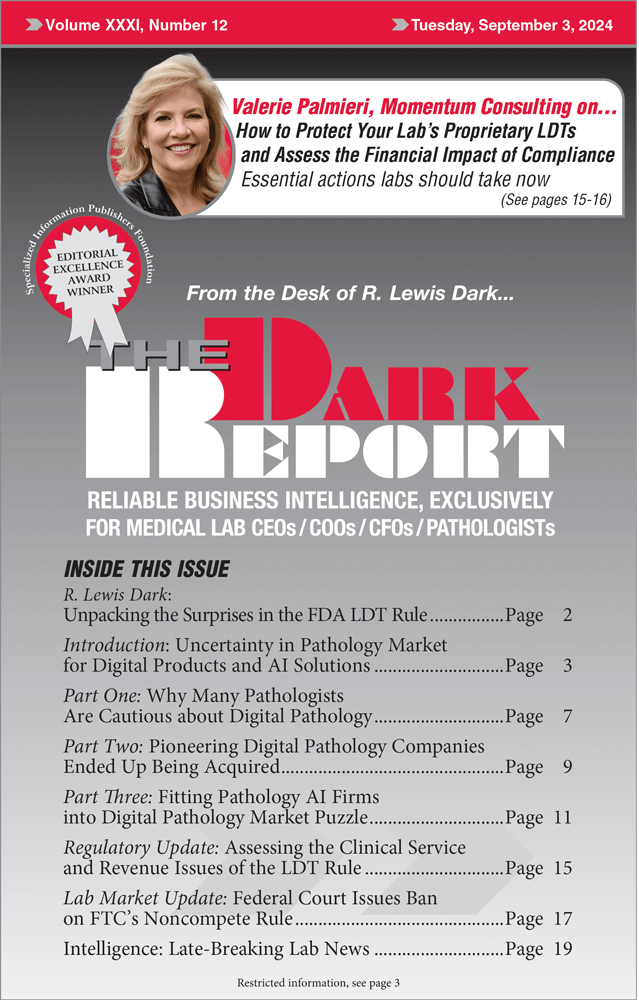
Volume XXXI, No. 12 – September 3, 2024
This special intelligence briefing—presented in three parts—identifies the factors retarding a faster adoption of digital pathology. Also, how to protect your lab’s proprietary LDTs and assess the financial impact of compliance.
See the full table of contentsHow Much Laboratory Business Intelligence Have You Missed?
Lab leaders rely on THE DARK REPORT for actionable intelligence on important developments in the business of laboratory testing. Maximize the money you make-and the money you keep! Best of all, it is released every three weeks!
Sign up for TDR Insider
Join the Dark Intelligence Group FREE and get TDR Insider FREE!
Never miss a single update on the issues that matter to you and your business.
Topics
- Anatomic Pathology
- Clinical Chemistry
- Clinical Laboratory
- Clinical Laboratory Trends
- Digital Pathology
- Genetic Testing
- In Vitro Diagnostics
- IVD/Lab Informatics
- Lab Intelligence
- Lab Marketplace
- Lab Risk & Compliance
- Laboratory Automation
- Laboratory Billing
- Laboratory Compliance
- Laboratory Equipment
- Laboratory Information Systems
- Laboratory Management
- Lean Six Sigma
- Managed Care Contracts
- Molecular Diagnostics
- Pathology Trends
- People
- Uncategorized
The Dark Report • 21806 Briarcliff Dr • Spicewood, TX 78669
Phone: 512-264-7103 • Toll Free Number: 800-560-6363
Email: info@darkreport.com
© 2024 The Dark Report. All rights reserved.

