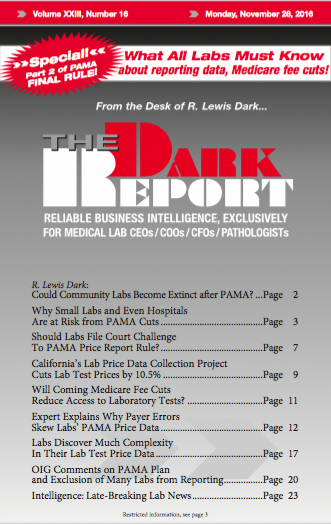
DON’T EXPECT IT TO BE EASY AND STRAIGHTFORWARD when reporting the prices of chemistry panels as the final rule for lab test market price reporting rule requires. Instead, labs should expect the process to be complex and troublesome. Also, labs should be concerned that Medicare officials have threatened to make deep cuts to chemistry panel …
Labs Discover Much Complexity In Their Lab Test Price Data Read More »
To access this post, you must purchase The Dark Report.