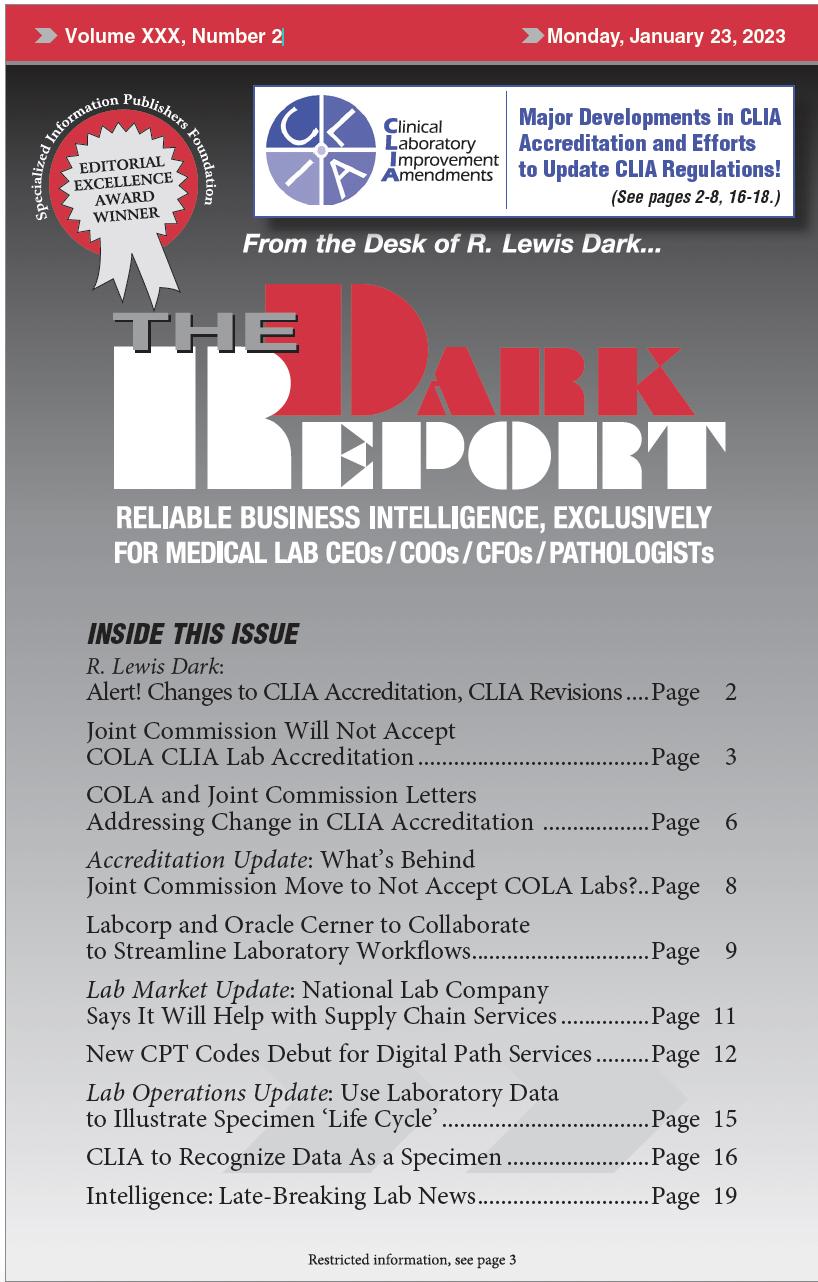
CEO SUMMARY: Discussions within the federal Clinical Laboratory Improvement Advisory Committee (CLIAC) are focusing on digital diagnostic data and clinical laboratory testing conducted remotely. CLIAC recommendations about these important topics may eventually be part of updates to CLIA, whose language has remained largely untouched since its inception in 1988. SWEEPING RECOMMENDATIONS ARE BEFORE FEDERAL CLINICAL […]
To access this post, you must purchase The Dark Report.