CEO SUMMARY: In the absence of public discussion, continued use of the “free testing” strategy by the nation’s more aggressive laboratory companies could trigger some unpleasant consequences that would affect all laboratories and pathology group practices. Five questions, presented here, illustrate how private and public healthcare payers might react to the ongoing use of “free …
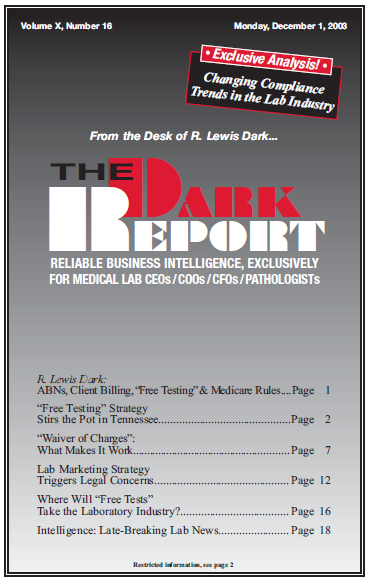
Where Will “Free Tests” Take the Lab Industry? Read More »
To access this post, you must purchase The Dark Report.