CEO SUMMARY: That famous phrase “everyone wants something for nothing” does not describe TennCare Select’s reaction to the “free testing” that Quest Diagnostics is performing for its beneficiaries. TennCare provides a real-world example of how this strategy can put a laboratory at odds with an important payer in a region. An experienced healthcare attorney assesses …
Lab Marketing Strategy Triggers Legal Concerns Read More »
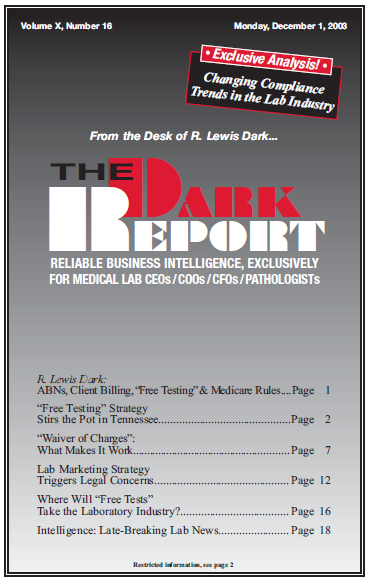
To access this post, you must purchase The Dark Report.