CEO Summary: When the Pathology Department at Scripps Memorial Hospital in La Jolla, California, was considering the purchase of a digital imaging system, it gained unlikely allies. Non-pathologist physicians participating in the department’s tumor boards advocated for the purchase after seeing a demonstration. Pathologists at Scripps are preparing for a future in which digital imaging …
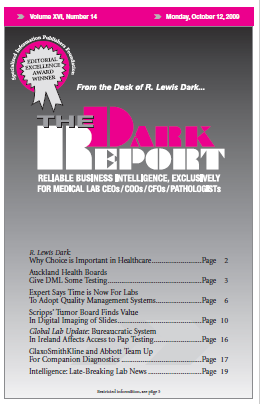
Scripps’ Tumor Board Finds Value in Digital Imaging of Slides Read More »
To access this post, you must purchase The Dark Report.