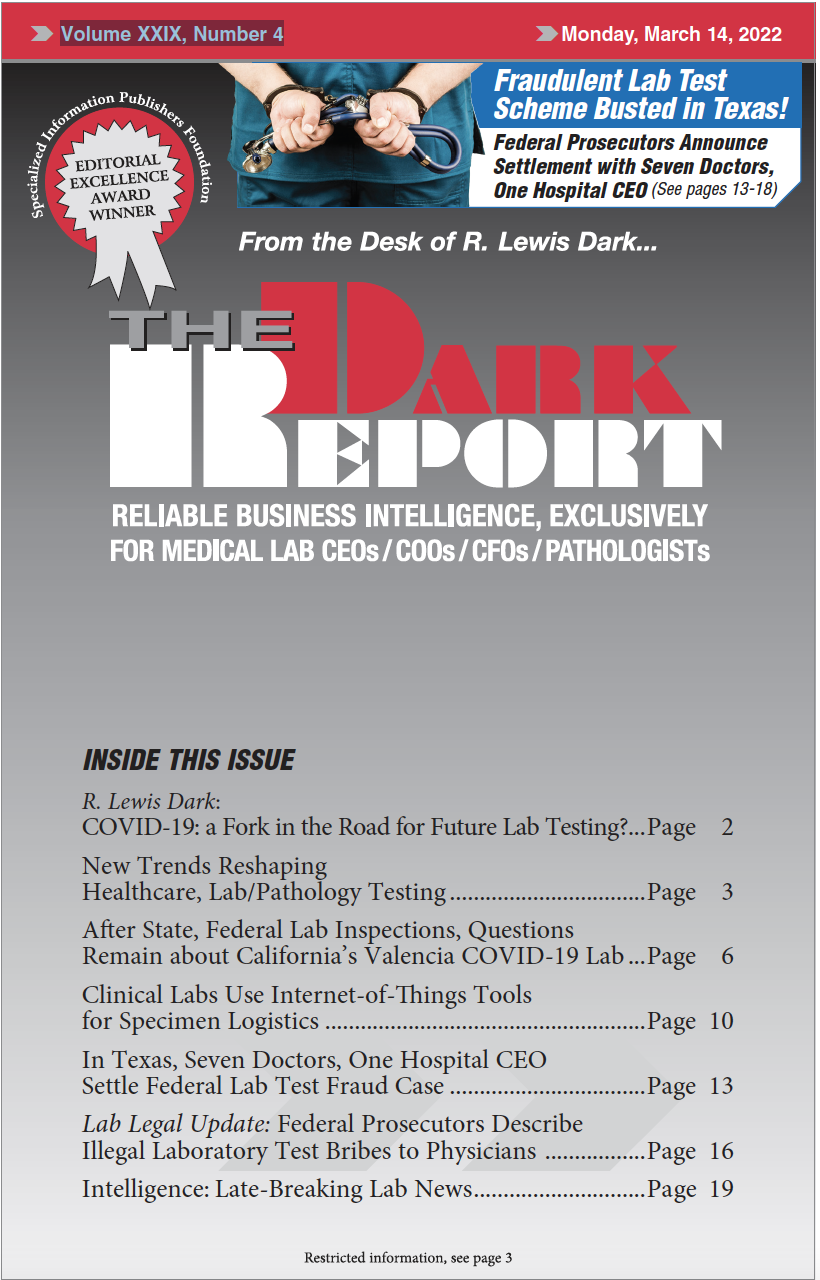
CEO SUMMARY: In January, a U.S. Attorney from East Texas announced that seven physicians and a hospital CEO had agreed to settle allegations of fraud involving the payment of bribes in exchange for lab test orders. This is a positive development for the clinical laboratory profession because it demonstrates that the federal Department of Justice …
Seven Doctors Settle Lab Test Fraud Case Read More »
To access this post, you must purchase The Dark Report.