IN RECENT DECADES, probably no sector of the U.S. healthcare system has seen the level of fraud and abuse that seems to pervade the clinical laboratory industry. The common perception is that illegal inducements between lab companies and referring physicians are rampant and federal prosecutors have failed to bring enough violators to justice to effectively …
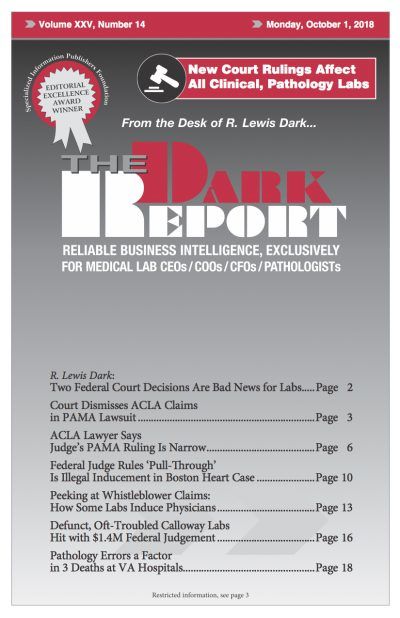
Peeking at Whistleblower Claims: How Labs Induce Physicians Read More »
To access this post, you must purchase The Dark Report.