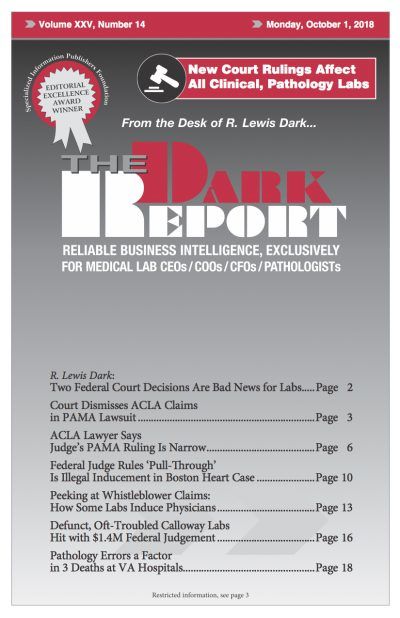
CEO SUMMARY: Many lab professionals were disappointed at the news that a federal judge dismissed the American Clinical Laboratory Association’s arguments in its lawsuit against the federal Department of Health and Human Services (HHS). In an interview, the ACLA’s lead lawyer on the case discussed the key issues and explained ACLA’s claims about how HHS …
ACLA Lawyer Says Judge’s PAMA Ruling Is Narrow Read More »
To access this post, you must purchase The Dark Report.