MEDICARE PART B CLINICAL LABORATORY FEE SCHEDULE CUTS mandated by PAMA continue to bite deeply. A new government report shows that during fiscal 2020, the Medicare program spent 15.9% less for lab tests, when COVID-19 test payments are excluded. The federal Department of Health and Human Services Office of Inspector General (OIG) recently released a …
Non-COVID Part B Lab Spend Declined by 15.9% in 2020 Read More »
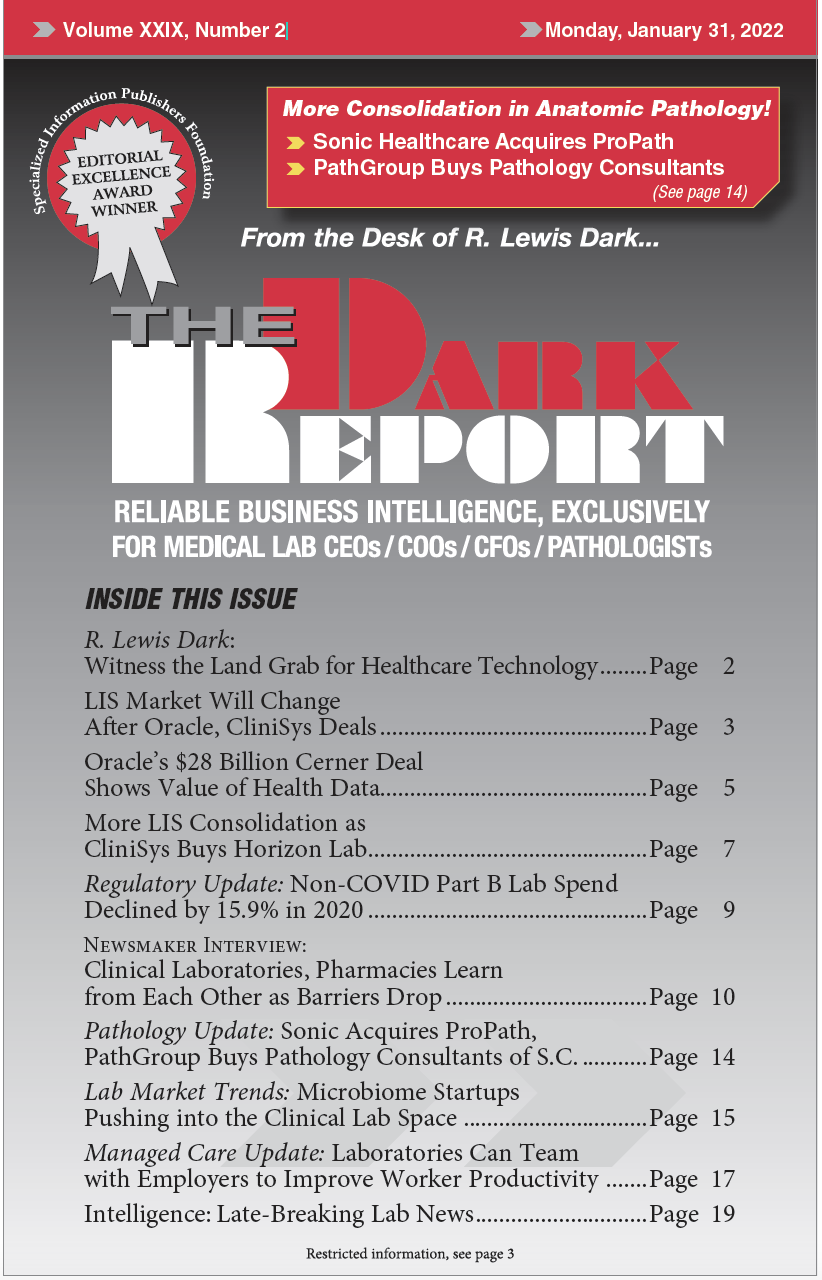
To access this post, you must purchase The Dark Report.