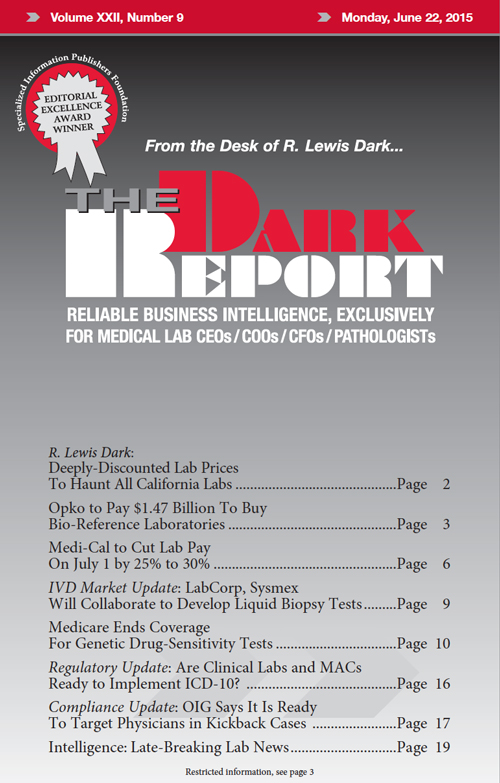
ARE CLINICAL LABORATORIES and pathology groups prepared for ICD-10? Or, perhaps a better question to ask is this: Are Medicare Administrative Contractors prepared to switch to ICD-10 on October 1?
To access this post, you must purchase The Dark Report.