TAG:
local coverage determinations
Smaller Labs Must Verify Z-code Arrangement with Lab Companies
By Virchow | From the Volume XXX, No. 12 – August 21, 2023 Issue
EDITOR’S NO…
Medi-Cal to Cut Lab Pay on July 1 by 25% to 30%
By Joseph Burns | From the Volume XXII NO. 9 – June 22, 2015 Issue
CEO SUMMARY: Since 2011, state officials in California have aggressively cut laboratory testing fees for Medi-Cal, the state’s Medicaid program. Now state officials say they will implement a new methodology next month for determining lab testing fees. The new methodology is based…
Are Clinical Labs and MACs Ready to Implement ICD-10?
By Robert Michel | From the Volume XXII NO. 9 – June 22, 2015 Issue
ARE CLINICAL LABORATORIES and pathology groups prepared for ICD-10? Or, perhaps a better question to ask is this: Are Medicare administrative contractors prepared to switch to ICD-10 on October 1? A recent survey of clinical laboratories and pathology groups by McKesson Corporation showed th…
April 28, 2014 Intelligence: Late Breaking Lab News”
By Robert Michel | From the Volume XXI NO. 6 – April 28, 2014 Issue
In recent years, a series of decisions involving molecular diagnostics tests made by Medicare officials and the Medicare Administrative Contractors (MACs) have caused much disruption in the clinical laboratory industry. In response to these developments, on April 16, the California Clinical L…
Price Cuts, Long Delays in Payment Are Expected
By Joseph Burns | From the Volume XIX No. 18 – December 31, 2012 Issue
CEO SUMMARY: In addition to a steep cut in the 88305 CPT code, anatomic pathology laboratories can expect cuts in the payment from Medicare for molecular and prostate biopsy testing. Two national experts in lab billing and reimbursement warn labs to expect confusion in how both public and…
2011’s Top 10 Lab Stories Point to a Busy 2012
By Robert Michel | From the Volume XIX No. 1 – January 9, 2012 Issue
CEO SUMMARY: Given the specific news stories that make up THE DARK REPORT’S list of the “Top Ten Lab Stories for 2011,” it might be said that 2011 was a rather quiet year overshadowed by anticipation of the coming reforms mandated by the Accountable Care Act of 2010. For the clinica…
ACLA Has its Say Regarding Molecular Dx Proposals
By Robert Michel | From the Volume XVIII No. 17 – December 19, 2011 Issue
CEO SUMMARY: It is not known how many public comments have been submitted to Palmetto GBA, the big Medicare carrier, in response to its published proposals to change how code stacked claims for genetic and molecular tests will be handled, effective February 27, 2012, for labs in Medicare …
Palmetto Execs Explain Molecular Test Policies
By Joseph Burns | From the Volume XVIII No. 16 – November 28, 2011 Issue
CEO SUMMARY: To create more transparency in the process clinical labs use to submit claims for genetic tests, molecular diagnostic tests, and for laboratory-developed tests (LDT), the nation’s largest Medicare Administrative Contractor (MAC) has proposed two new local coverage determina…
Palmetto GBA Announces Molecular Test Registry
By Joseph Burns | From the Volume XVIII No. 16 – November 28, 2011 Issue
CEO SUMMARY: Palmetto GBA, the nation’s largest Medicare Administrative Contractor (MAC), is asking labs in the J1 jurisdiction to submit applications for each molecular test they run. Molecular assays will receive a unique five-digit alpha-numeric identifier (Z-code) that will be enter…
Economics of Lab Testing to Be Challenged
By R. Lewis Dark | From the Volume XVIII No. 15 – November 7, 2011 Issue
BY ANY MEASURE, 2012 IS SHAPING UP TO BE A YEAR OF MAJOR CHANGE for healthcare and the clinical laboratory testing industry. Unfortunately, an early reading of the tea leaves indicates that the outcomes are not likely to be favorable for most clinical laboratories and anatomic pathology groups. Letâ…
CURRENT ISSUE
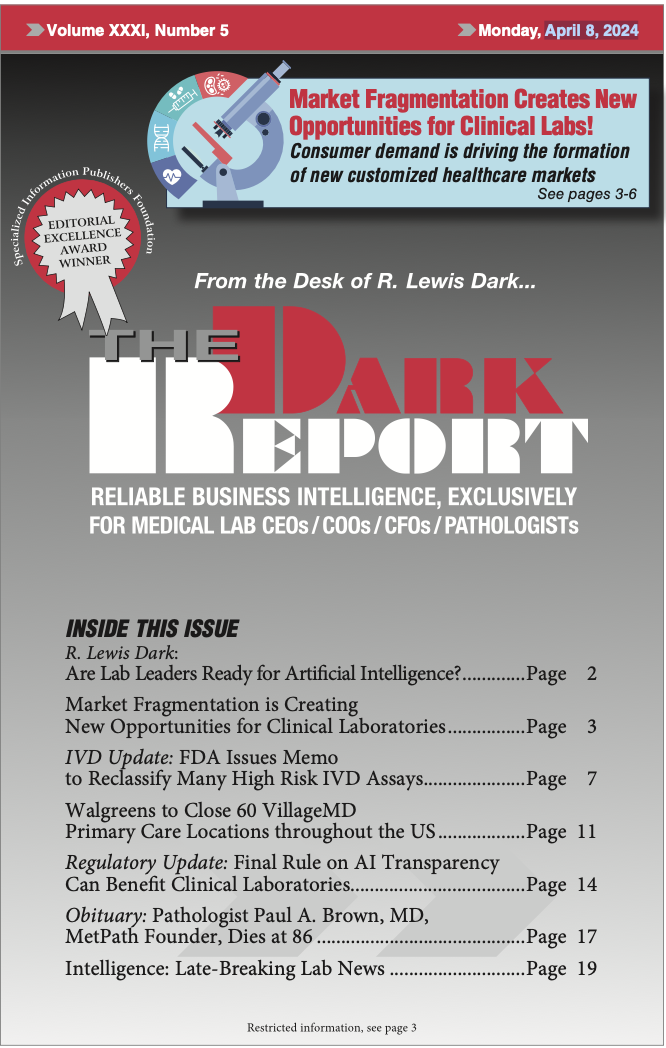
Volume XXXI, No. 5 – April 8, 2024
The fragmentation of consumer markets is reflected in clinical lab services, and The Dark Report examines this trend and how it will impact labs in the coming years. Also, The Dark Report notes that the FDA has issued a controversial memo to reclassify many high-risk IVD assays.
See the full table of contentsHow Much Laboratory Business Intelligence Have You Missed?
Lab leaders rely on THE DARK REPORT for actionable intelligence on important developments in the business of laboratory testing. Maximize the money you make-and the money you keep! Best of all, it is released every three weeks!
Sign up for TDR Insider
Join the Dark Intelligence Group FREE and get TDR Insider FREE!
Never miss a single update on the issues that matter to you and your business.
Topics
- Anatomic Pathology
- Clinical Chemistry
- Clinical Laboratory
- Clinical Laboratory Trends
- Digital Pathology
- Genetic Testing
- In Vitro Diagnostics
- IVD/Lab Informatics
- Lab Intelligence
- Lab Marketplace
- Lab Risk & Compliance
- Laboratory Automation
- Laboratory Billing
- Laboratory Compliance
- Laboratory Equipment
- Laboratory Information Systems
- Laboratory Management
- Lean Six Sigma
- Managed Care Contracts
- Molecular Diagnostics
- Pathology Trends
- People
- Uncategorized
The Dark Report • 21806 Briarcliff Dr • Spicewood, TX 78669
Phone: 512-264-7103 • Toll Free Number: 800-560-6363
Email: customerservice@darkintelligencegroup.com
© 2022 The Dark Report. All rights reserved.

