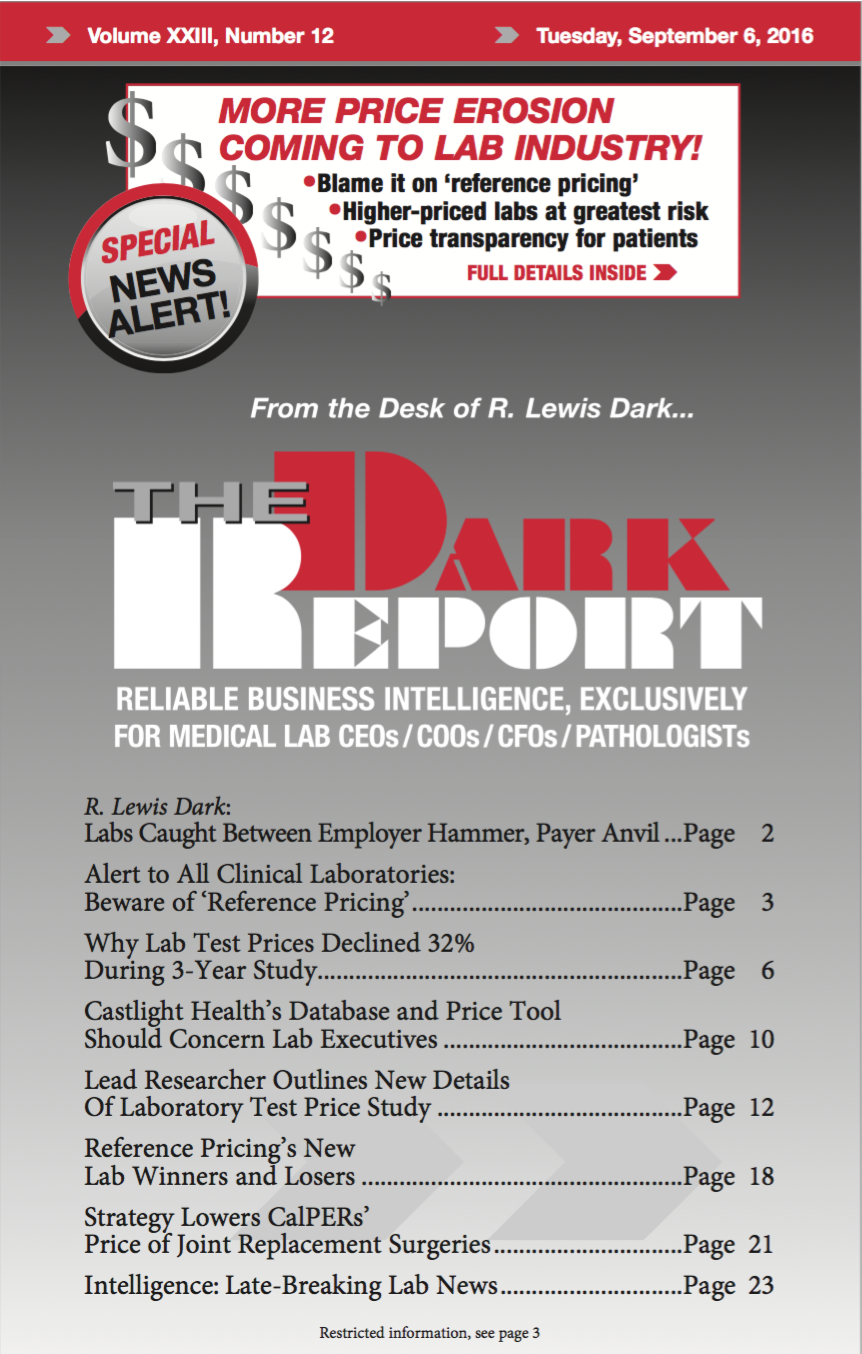
CEO SUMMARY: “Reference pricing” does not refer to how a lab negotiates prices with its reference lab! Rather, reference pricing describes a specific approach to health plan benefits that incentivizes the consumer to choose lower-cost providers while allowing that consumer to still use a higher-priced provider, so long as that consumer pays the additional costs …
Alert to All Labs: Beware Of ‘Reference Pricing’ Read More »
To access this post, you must purchase The Dark Report.