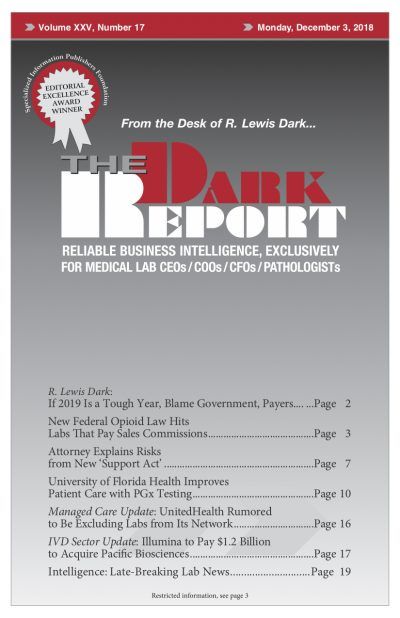
IN RECENT DAYS, RUMORS HAVE SURFACED that UnitedHealthcare has begun to terminate the contracts it holds with a number of regional and non-national clinical laboratories. This news surfaced just as The Dark Report went to press. Given its importance to the clinical laboratory industry, we wanted to alert lab executives and pathologists to this development …
UnitedHealth Rumored to Be Excluding Labs from Its Network Read More »
To access this post, you must purchase The Dark Report.