CEO SUMMARY: Efforts to help physicians improve their utilization of clinical lab tests paid big dividends at the Johns Hopkins Bayview Medical Center in Baltimore, Maryland. Working collaboratively, physicians and the clinical lab team identified overused or needless cardiac biomarker tests, then designed interventions to improve how physicians used these tests. The result was a …
Doctors at Johns Hopkins Improve Lab Test Utilization Read More »
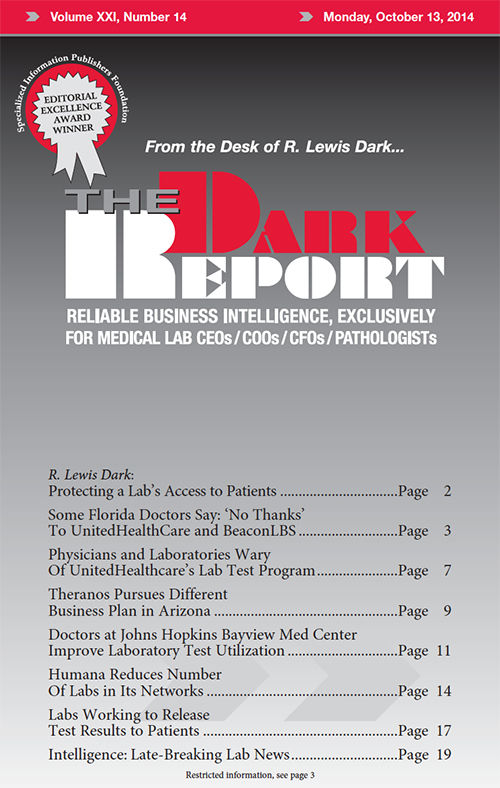
To access this post, you must purchase The Dark Report.