CEO SUMMARY: Some Florida physicians are declaring their intent to leave UnitedHealthcare’s network because they find the insurer’s new BeaconLBS laboratory benefit management system to be time consuming and onerous. The defections come as the program goes through a soft launch that began on October 1. Apparently in response to physician complaints, UHC announced a …
FL Docs Say: ‘No Thanks’ to UHC and BeaconLBS Read More »
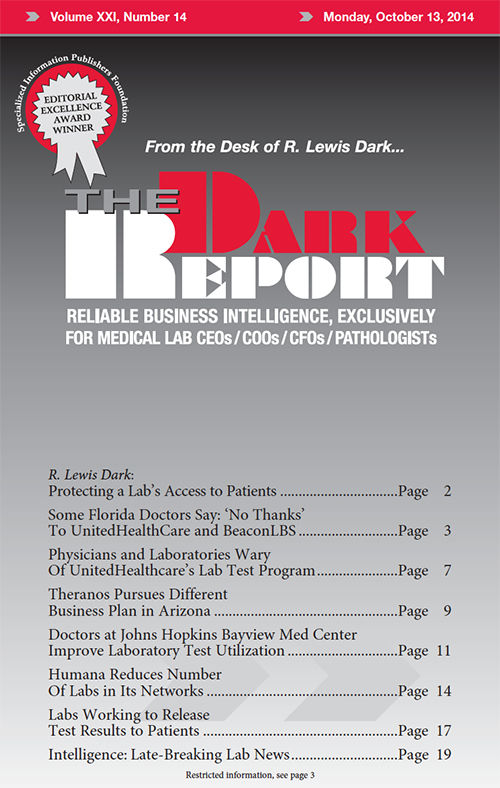
To access this post, you must purchase The Dark Report.