CEO SUMMARY: Providers seem to have a natural distrust of health insurers, particularly when payers introduce new programs with the stated purpose of improving quality and ensuring that physicians deliver evidence-based medicine. Doctors serving members of UHC’s HMO plans in Florida are told by UHC that it wants to improve the quality of lab test …
Physicians and Labs Wary of United’s Lab Test Program Read More »
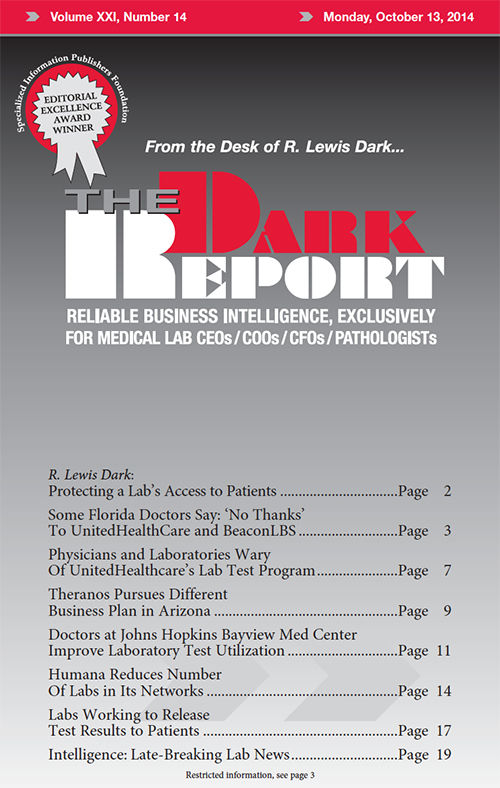
To access this post, you must purchase The Dark Report.