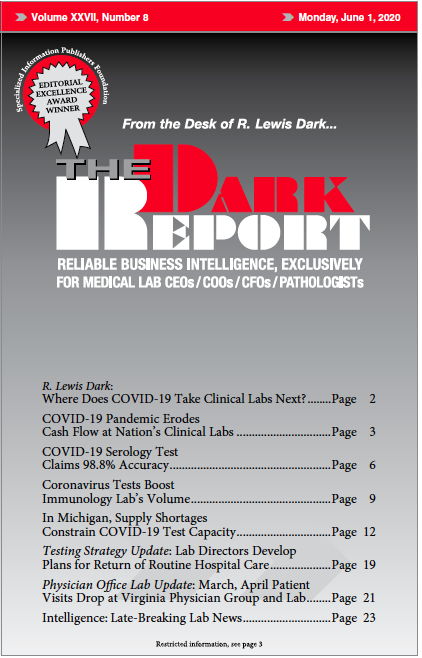
CEO SUMMARY: When it announced its new antibody test for the novel coronavirus SARS-CoV-2 on May 3, Roche Holdings explained that its sensitivity level after 14 days was 100%, which is an important point to understand about the test. When assessing Roche’s claims, two experts agreed that the test performs exceptionally well. Abbott Laboratories also reported high performance levels for its …
COVID-19 Serology Test Claims 98.8% Accuracy Read More »
To access this post, you must purchase The Dark Report.