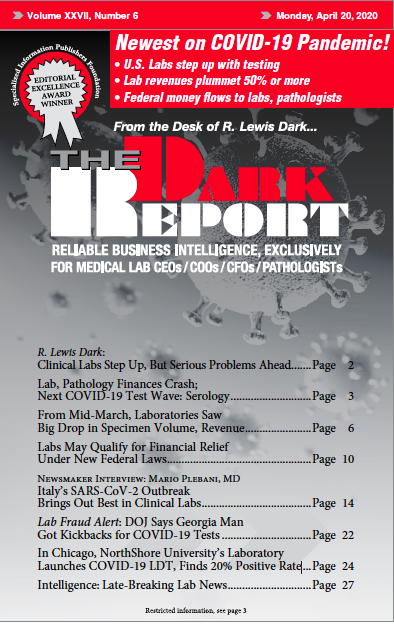
CEO SUMMARY: After seeing the novel coronavirus spread quickly in China, staff in the Department of Pathology and Laboratory Medicine developed a test to identify the pathogen in patients in Chicago and its suburbs. With the CDC’s assay in hand, it started work on its own lab-developed test. In early April, the lab tested more than 10,000 patients and approximately 20% […]
To access this post, you must purchase The Dark Report.