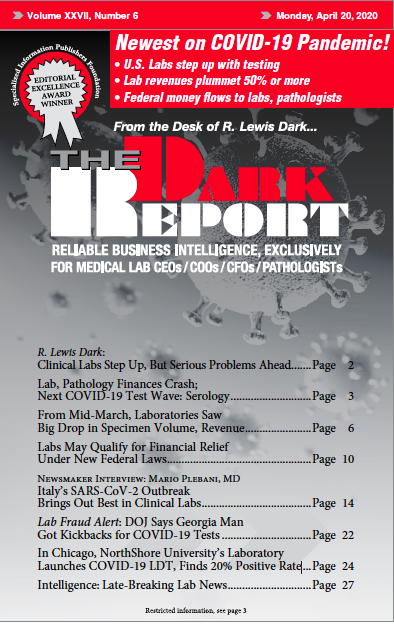
CEO SUMMARY: Italy was one of the first countries outside of China to experience an explosive outbreak of COVID-19 and its northern provinces were hit hardest by this novel coronavirus. In this exclusive interview with THE DARK REPORT, internationally-known pathologist Mario Plebani, MD, discusses how his clinical laboratory in Padova responded to the pandemic in the Veneto Region. Second of …
Italy’s SARS-CoV-2 Outbreak Brings Out Best in Clinical Labs Read More »
To access this post, you must purchase The Dark Report.