CEO SUMMARY: Probably no state has seen a faster transition to ACOs, medical homes, and other types of integrated clinical care organizations than Arizona. Recognizing that this change created a new opportunity to add more value with clinical lab testing services, Sonora Quest Laboratories (SQL) developed an enterprise-wide master patient index. This gives SQL the …
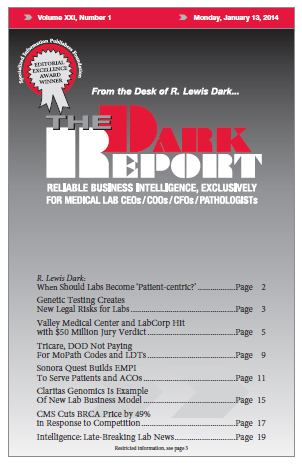
Sonora Quest Builds EMPI To Serve Patients and ACOs Read More »
To access this post, you must purchase The Dark Report.