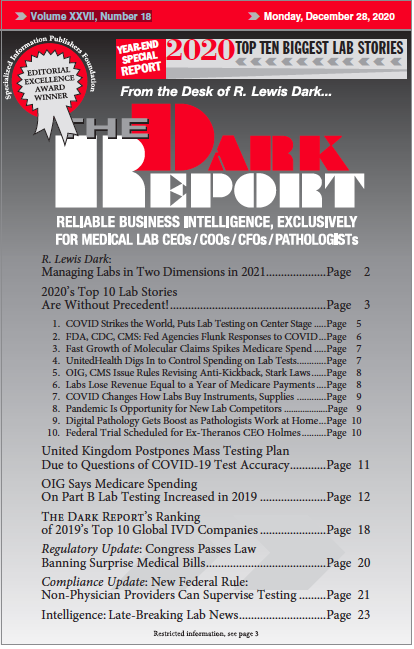
This is an excerpt of a 3,689-word article in the December 28, 2020 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. CEO SUMMARY: There are several surprises in The Dark Report’s list of the Top 10 Lab Stories for 2020. Despite the SARS-CoV-2 pandemic dominating …
Top 10 2020 Lab Stories Are about More than Just COVID-19 Read More »
To access this post, you must purchase The Dark Report.