Starting Jan. 1, 2022, out-of-network clinical laboratories may no longer be allowed to bill patients for lab tests performed in certain settings under a law both houses of Congress passed on Dec. 21. The COVID relief bill includes a ban on unexpected medical bills from some out-of-network providers, such as clinical laboratories, anatomic pathologists, anesthesiologists, …
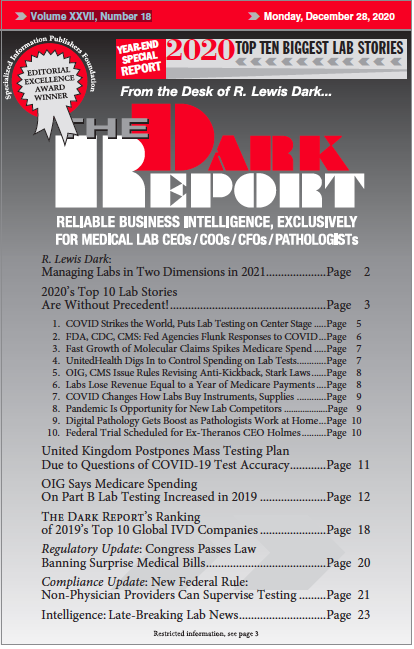
Congress Passes Bill to Ban Surprise Medical Bills Read More »
To access this post, you must purchase The Dark Report.