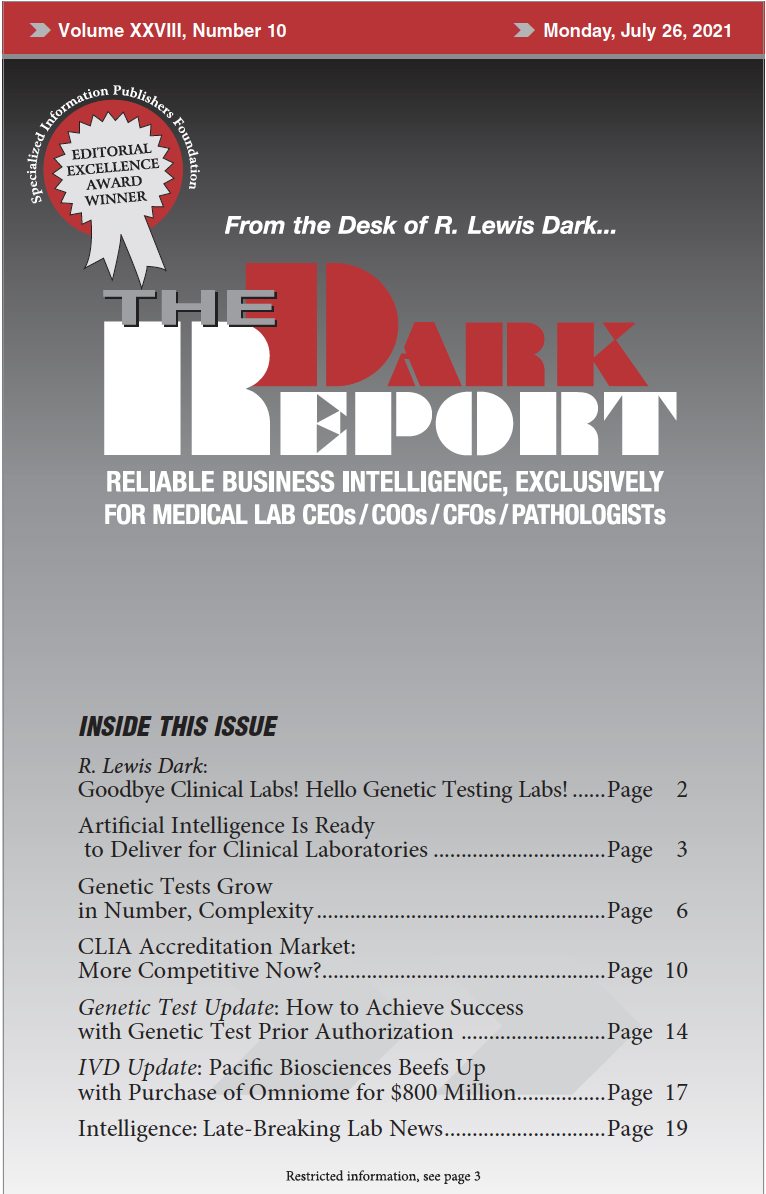
This is an excerpt of a 1,333-word article in the July 26, 2021 issue of THE DARK REPORT (TDR). The full article is available to members of The Dark Intelligence Group. CEO SUMMARY: Getting paid for genetic testing continues to be a challenge. This is true for both payers and the labs that perform the …
Genetic Testing Continues to Grow in Volume and Complexity Read More »
To access this post, you must purchase The Dark Report.