CEO SUMMARY: Getting paid for genetic tests continues to be a challenge. This is true for both payers and the labs that perform the tests. Even physicians are dissatisfied with the status quo because they must deal with patients unhappy about the high cost of genetic tests. The problem is likely to get worse before …
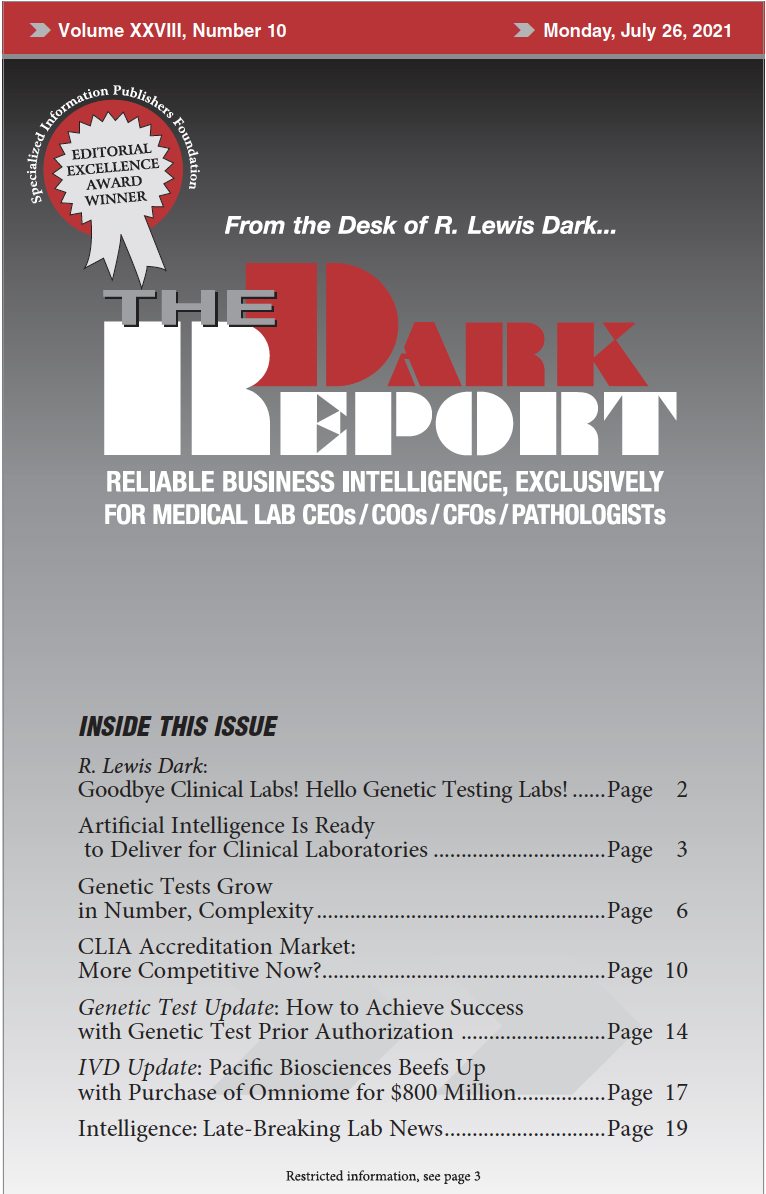
Genetic Tests Grow in Number, Complexity Read More »
To access this post, you must purchase The Dark Report.