TAG:
private payer
TOP 10 LAB STORIES OF 2017
By Robert Michel | From the Volume XXIV No. 17 – December 11, 2017 Issue
1. CMS Sticks by Decision to Deeply Cut Medicare Part B Lab Test Fees SHORT OF A MIRACLE, the clinical laboratory industry is less than three weeks from the single most financially-disruptive event of the past 30 years. On Jan. 1, the federal Centers for Medicare and Medicaid Service…
ACLA Sues HHS over Market Price Study, Fee Cuts
By R. Lewis Dark | From the Volume XXIV No. 17 – December 11, 2017 Issue
IT’S A LONG-AWAITED DEVELOPMENT! Today, a federal lawsuit was filed against the Department of Health and Human Services (HHS) by the American Clinical Laboratory Association (ACLA). The lab association is asking a federal judge to review specific actions taken by …
ACLA hits Medicare fee schedule cuts with lawsuit
By Mary Van Doren | From the Volume XXIV No. 17 – December 11, 2017 Issue
This is an article from the Dec. 11, 2017 issue of THE DARK REPORT. The complete article is available for a limited time to all readers. This article plus a full analysis of 2017 developments in the PAMA process are available at all times to paid members of the Dark Int…
Tougher Times Ahead as Labs React to Fee Cuts
By Joseph Burns | From the Volume XXIV No. 16 – November 20, 2017 Issue
CEO SUMMARY: Just as Nero is reputed to have fiddled while Rome burned, officials at CMS seem to be doing their own fiddling as their planned deep price cuts to Medicare Part B lab tests could begin driving lab companies out of business. In recent weeks, the owners of two lab companies de…
Fla. Lab Sells to Labcorp, But Keeps Nursing Homes
By Joseph Burns | From the Volume XXIV No. 16 – November 20, 2017 Issue
CEO SUMMARY: Vista Clinical Diagnostics of Clermont, Fla., is betting big on the nursing home sector just when many labs serving nursing homes are worried about steep Medicare cuts coming Jan. 1. After selling its physician office referral testing, 35 patient service centers, and a mobile…
Is the Worm Turning in Favor of Hospital Labs?
By R. Lewis Dark | From the Volume XXIV No. 16 – November 20, 2017 Issue
SINCE THE MID-1990S, HOSPITAL OUTREACH LABORATORY PROGRAMS have lost market share steadily to the nation’s biggest public lab companies. In these two decades, public lab companies traded deeply-discounted lab test prices to health insurers in exchange for exclusive network provider status. Then, a…
Some Labs Performing ADLTs May See Increased Medicare Fees
By Joseph Burns | From the Volume XXIV No. 15 – October 30, 2017 Issue
MIXED IN THE BAD NEWS concerning the proposed Clinical Laboratory Fee Schedule for 2018, there is some good news regarding what the federal Centers for Medicare and Medicaid Services proposes to pay for certain advanced diagnostic tests. After analyzing the proposed fee schedule, …
Looming CMS lab fee schedule cuts unite AMA, AHA and labs in opposition
By Mary Van Doren | From the Volume XXIV No. 14 – October 9, 2017 Issue
This is an excerpt from a 1,237-word article in the Oct. 8, 2017 issue of THE DARK REPORT. The complete article is available for a limited time to all readers, and available at all times to paid members of the Dark Intelligence Group. CEO SUMMARY: In what m…
AMA, AHA Join Labs to Request Delay, Fix
By Robert Michel | From the Volume XXIV No. 14 – October 9, 2017 Issue
CEO SUMMARY: In what may be a first for the clinical lab industry, the American Medical Association and the American Hospital Association joined with 20 other healthcare associations to ask CMS Administrator Seema Verma to address the problems with the CMS proposal involving Medicare Part B f…
XIFIN CEO White Analyzes Medicare 2018 Fee Cuts
By R. Lewis Dark | From the Volume XXIV No. 14 – October 9, 2017 Issue
CEO SUMMARY: If the draft lab rates that CMS published Sept. 22 for the Clinical Laboratory Fee Schedule for 2018 go into effect Jan. 1 as proposed, then clinical labs will see a cut of 28% in what they get paid for the top 20 most common tests, according to a recent analysis. The rates t…
CURRENT ISSUE
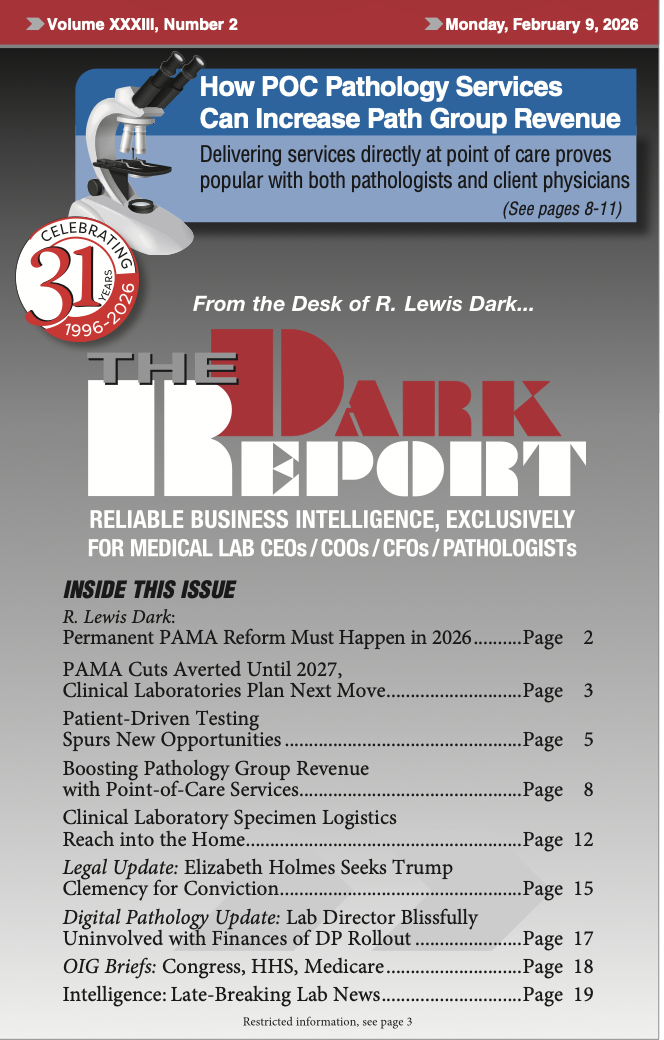
Volume XXXIII, No. 2 – February 9, 2026
Congress has once again delayed cuts to test reimbursement rates under PAMA, this time until Jan. 1, 2027. Laboratory professionals are urged to lobby Congress to pass the RESULTS act to solve the PAMA cuts problem permanently. Also, patient-driven testing is spurring new opportunities.
See the full table of contentsHow Much Laboratory Business Intelligence Have You Missed?
Lab leaders rely on THE DARK REPORT for actionable intelligence on important developments in the business of laboratory testing. Maximize the money you make-and the money you keep! Best of all, it is released every three weeks!
Sign up for TDR Insider
Join the Dark Intelligence Group FREE and get TDR Insider FREE!
Never miss a single update on the issues that matter to you and your business.
Topics
- Anatomic Pathology
- Clinical Chemistry
- Clinical Laboratory
- Clinical Laboratory Trends
- Digital Pathology
- Genetic Testing
- In Vitro Diagnostics
- IVD/Lab Informatics
- Lab Intelligence
- Lab Marketplace
- Lab Risk & Compliance
- Laboratory Automation
- Laboratory Billing
- Laboratory Compliance
- Laboratory Equipment
- Laboratory Information Systems
- Laboratory Management
- Lean Six Sigma
- Managed Care Contracts
- Molecular Diagnostics
- Pathology Trends
- People
- Uncategorized

